- Date:2020-01-07
About Radiology
The Department of Radiology was founded in 1953, located in the bungalow on the east side of Huamei Building, with only one 100mA semi-rectified X-machine made in Hungary, and moved to the south side of the new outpatient clinic of the East Hospital in June 1967, with one domestically made 58-200mA fluoroscopy machine and one KE200mA film machine, and was moved to the Imaging Building in March 1998, with the introduction of Hitachi 1000mA remote-controlled gastrointestinal machine and 630mA high-frequency suspension film machine, and imported fully automated film processing machine. In March 1998, it moved into the imaging building and introduced Hitachi 1000mA remote-controlled gastrointestinal machine and 630mA high-frequency suspension radiograph, and imported automatic film processing machine. At present, the department has developed into a new type of discipline integrating diagnosis and treatment, scientific research and teaching and possessing large-scale modern imported equipments, and was awarded ‘Key Discipline of Liaocheng City’ and named ‘Model Department of Liaocheng City’ in 2005. For many years, the department has been responsible for the internship and teaching of Taishan Medical College and other universities, and has been designated as the training base of Shandong Province's ‘360 Project’ and ‘1127 Project’.
There are 26 professional and technical personnel in the department, including 1 senior, 7 vice senior and 10 intermediate titles. The staff at all levels went to Tianjin, Beijing, Shanghai, Nanjing, Jinan, Yantai and other provincial hospitals for further training and study, and introduced and carried out more than 30 new technologies, and won three second-class prizes for scientific and technological progress in Liaocheng City and sixteen third-class prizes; two first-class prizes for scientific and technological progress at Taishan Medical College, two third-class prizes, and sixteen scientific and technological progress prizes at the hospital. More than 100 papers have been published in magazines above the provincial level, and eight imaging monographs have been published;
There are ten sets of imported equipments, and in 2010, a huge amount of money was introduced into the U.S. Kodak 7500 double-plate DR, also known as the ‘transcendent new generation of intelligent digital flat-panel radiological system,’ 7 seconds after the ingestion of the film, not only the image is rich in level and clear, which can greatly shorten the patient's waiting time, and is now put into use. U.S. GE800mA mA high-frequency suspended film machine with multifunctional universal bed, not only convenient for patients to check and clear images; Japan-made Zhaori brand oral panoramic X-ray machine is the first of its kind in the region, which can clearly show the whole picture of the oral cavity and teeth, in addition to meet the diagnosis of the disease, especially for children's teeth, school type has a guiding role; the U.S. Gold Standard Breast Machine can show the early stage of breast cancer. Germany AGFA fourth-generation computer digital imaging system CR, the machine is equipped with paediatric, breast, oral panoramic software, 5303 type of the most advanced laser camera, the real digital photography, improve the quality of the image for the patient's diagnosis to provide security. Japan Toshiba Winscope2000 digital gastrointestinal machine, the image is clear and can be continuously and dynamically captured, which can meet the needs of a variety of inspections. 2000 introduction of Japan Toshiba CAS-8000V suspended angiography DSA is the first one in northwestern Shandong Province, the machine has the following characteristics: (1) dual-track C-arm system can be used to carry out angiography of all parts of the body; (2) 1 million-pixel CCD digital camera; (3) 1 million-pixel digital camera; (4) 1 million-pixel CCD digital camera. (2) 1,000,000 pixel CCD digital photography system, 24-48 frames per second image acquisition is paid to ensure the clarity of the image under the dynamic. 2011 the introduction of Siemens flat detector DSA, Siemens flat detector DSA angiography machine as the world's most advanced German Siemens suspended flat detector angiography system, put into the clinical application for Cardiac intervention, neurological intervention, four-week intervention and diagnosis and treatment of diseases related to all parts of the body and organs, especially for the diagnosis and examination of large blood vessels and blood vessels of various systems and their lesions, it has replaced ordinary angiography, making endovascular and extravascular interventions quicker and safer. At the same time, it also has the following characteristics:
1, Volume reconstruction Dual-Volume, i.e. double volume reconstruction of bone and blood vessels, no overlapping of bone and soft tissue shadow, making the display of blood vessels and their lesions more intuitive;
2, iPilot Dynamic, i.e., real-time superimposition of fluoroscopic images and 3D images, which is helpful for peripheral intracranial aneurysms;
3, C-arm automatic three-dimensional reconstruction after position tracking and three-dimensional reconstruction image real-time tracking of the C-arm in different positions, this function is very meaningful for neurological intervention, intracranial aneurysm, to improve its diagnosis rate, but also clear judgement of cerebral arterial stenosis.
4, CT-like function, the blood vessels of intrahepatic tumour super-selective significance (positioning), craniocerebral CT also plays a monitoring role, craniocerebral CT can be observed at any time during the operation with or without bleeding and haemorrhage foci localisation without the need to move the patient to the CT room. In addition, DSA can not only clearly diagnose vascular lesions in the chest and abdomen, but also clearly show the blood supply arteries of liver tumours, and its CT-like function makes it more accurate for radiological interventions, especially for the localisation of intrahepatic tumours. Meanwhile, this device is more meaningful for the diagnosis of vascular lesions in the head and neck, especially intracranial aneurysm, which can clearly show the neck of the aneurysm, which is conducive to the choice of treatment and the determination of the treatment plan.
At the end of September, the Department of Neurosurgery, in collaboration with the Department of Critical Care and the Department of Anaesthesiology, operated on a patient with aneurysm embolisation. This case of intracranial aneurysm intervention was the first of its kind in our hospital, and was successful with good results. During the procedure, the C-arm was rapidly rotated to collect data for reconstruction and imaging, and after the formation of three-dimensional vascular images, the C-arm stent was automatically tracked with the rotation of the three-dimensional image, which allowed the observation of the embolisation effect, especially the embolisation of the cerebral aneurysm, the presence of re-bleeding, and the display of the position of the micro-spring coil, which was more clear and intuitive, and was helpful for the guidance of the catheter and the guidewire, which was more likely to be sent to the diseased part of the vessel, and was able to completely and densely fill the aneurysm, and to completely fill the aneurysm. The application of this machine solves the inconvenience of CT examination in the process of interventional therapy and facilitates the treatment. The real-time image reproduction and clear image of this machine can make various interventional diagnosis and treatment of our hospital to a higher level. 2003 built PACS system and gradually improved, realised the digitalization of image reading and storage, and started the computer printing and storage of the report card at the same time, at present, the images can be accessed at will between the imaging departments (Pradiography, CT, MRI, ECT, ultrasonography), and at the same time, established the clinical terminal workstation, patients can have a few minutes of workstation after the examination, and can have a few minutes of workstation after the examination. At the same time, a clinical terminal workstation has been established so that patients can view their image data on the workstation a few minutes after the examination.
Scope of work of the Department of Radiology
The radiology department carries out projects such as filming of various parts (all digitalized), imaging examinations of various systems, such as barium meal of the digestive tract, barium enema examination, rectal defecation imaging, uterine tubal imaging and arterial and venous angiography, etc. It is in a leading position in the region and surrounding counties and cities. At the same time, we have carried out interventional diagnosis and treatment of various parts of the body;
1、 Image-guided percutaneous lung aspiration biopsy to diagnose the nature of masses in the lungs; aspiration biopsy to diagnose bone and muscle lesions has been completed in more than 200 cases every year.
2. Interventional therapy for middle and late stage malignant tumors, interventional catheter therapy is to puncture the artery percutaneously, introduce the catheter into the artery to find the blood supplying artery of the tumor, and then inject the drugs into the lesion area directly through the catheter, and the concentration of the drugs in the local area can be increased by 10-30 times, which can directly kill the tumor cells, and thus achieve the purpose of treating the tumor. Especially, the interventional therapy for liver cancer and lung cancer achieves the purpose of reducing pain, prolonging life and improving quality of life, and treats more than 30 times of patients every year without any error or accident.
3. Interventional lysis treatment for ischemic necrosis of femoral head, through the catheter to dissolve the thrombus, activate blood and promote bone repair drugs into the blood supply artery of the femoral head, dissolve its artery, dredge its vein, from the root of the treatment of this disease, achieved remarkable curative effect, and won the Municipal Scientific and Technological Achievement Progress Prize. It has attracted patients from Henan, Hebei and neighboring counties to treat the disease, and has been highly evaluated.
4、 Memory stent placement for treatment of esophageal anastomotic stenosis, esophageal cancer that can not eat, stenosis after radiotherapy and esophageal tracheal leakage, and endovascular stent placement for treatment of peripheral vascular stenosis have achieved immediate results.
5、 Interventional minimally invasive treatment of lumbar intervertebral disc herniation: on the basis of percutaneous puncture lumbar intervertebral disc aspiration, we have successively carried out transabdominal puncture lumbar intervertebral disc extraction and percutaneous puncture lateral approach lumbar intervertebral disc extraction. Under the premise of selecting good indications, this technology can cure lumbar disc herniation radically, with the characteristics of small trauma, high safety, fast recovery and low cost, and nearly 200 cases have been completed so far, all of which have achieved therapeutic effects.
But the special feature: help you realize your dream of becoming a mother Ideal test for infertility patients
-Hysterosalpingogram with imported ultra-liquidized iodized oil
A Why do we need a hysterosalpingogram?
Tubal disease is the main cause of women's infertility. Hysterosalpingography can visualize the shape of the uterus and whether the tubes are open, not open or obstructed, observe whether there are adhesions, fluid accumulation and inflammation, and then treat the symptoms to help infertility patients realize the dream of being a mother as soon as possible.
II What are the advantages of hysterosalpingography with imported ultra-liquefied iodized oil?
Ordinary iodized oil has high viscosity, high irritation, and clear contrast, with the disadvantage of slow absorption and easy formation of granuloma. Water-soluble iodized contrast medium, with lower viscosity and high irritation, can be absorbed and discharged from kidneys, with the disadvantage of fast disappearance and lack of clarity of development. Imported super-liquefied iodized oil can have the advantages of both, low viscosity, no irritation, clear imaging, because of its super-liquefied, so the flow rate is faster than ordinary iodized oil, easy to be absorbed. At the same time, it also has the functions of sterilization, improving the mucus environment of cervical canal and reducing the phagocytosis of sperms by mononuclear cells. Because there is a certain pressure when injecting super-liquefied iodized oil for imaging, some patients can make the fallopian tube open and get pregnant, and the Reproductive Center can help them to get pregnant according to different situations after the diagnosis is clear and all of them have achieved satisfactory results.
The use of imported ultra-liquefied iodized oil as a contrast agent, and combined with digital imaging equipment continuous dynamic image acquisition for the whole process of hysterosalpingography, can be comprehensive dynamic observation of the whole picture of the uterus and fallopian tubes, clear pathology because of the diagnosis and treatment to provide a guarantee.
III What are the indications and precautions for hysterosalpingography?
Indications: secondary or primary infertility, to know the uterine morphology, whether the fallopian tubes are patent and the reasons for the impassability.
Contraindications: history of iodine allergy, hyperthyroidism, renal insufficiency, asthma and active tuberculosis, acute or subacute pelvic inflammatory disease, body temperature above 37.5°.
Imaging time: the 3rd-7th day after menstruation. Precautions: Avoid sexual intercourse and deep water pelvic bath for 3 days before and 2 weeks after the imaging. Take oral antibiotics for 3-5 days after imaging.


During Hysterosalpingography Normal presentation of hysterosalpingography


Bilateral tubal incompetence 24-hour review of bilateral hydrosalpinx
Specialist: An Xianghong 13562062334
Gao Xijie 13963512558
Zhang Jucai 13869512905
Li Menglei 15966272822
Do you know about imaging for constipation?
When it comes to "constipation", people think that it is difficult to defecate with dry stools, in fact, at present, the medical science collectively refers to the functional exit disorder as "constipation", and people know very little about how to check, how to diagnose, and how to treat it.
◆What can cause constipation?
According to the cause of the lesion, it can be divided into primary constipation and secondary constipation.
◇ Primary constipation: refers to the anatomical abnormalities and organic lesions of the large intestine and anal canal, and the lesions of organs outside the intestinal canal, such as pressure on the intestinal tract, which cause the slow running of faeces or obstruction of discharge: common ones are congenital megacolon, colorectal tumour, intestinal adhesion and narrowing, anal fissure, anal sinusitis, and stenosis of the anal canal, and so on.
◇ Secondary constipation: refers to the clinical manifestations mainly constipation, no organic lesions by various examinations. The causes are (1) mental constipation: excessive tension, neurosis, neurological disorders, etc.. (2) Laxative constipation:. (3) Drug constipation: analgesics, acid-forming drugs, antihypertensive drugs, antipsychotics. (4) Functional outlet obstruction constipation: anterior rectal protrusion, rectal mucosal prolapse, internal condylomata, perineal descent, pelvic floor hernia, pelvic floor loss of flaccidity and so on.
◇Primary constipation is preferred to gas barium enema examination. Secondary constipation is preferred to be examined by simulated rectal defecography (rectal defecography). For colon slow transmission constipation, examination with colon transmission test is preferred.
◆What are the common tests?
Simulated rectal defecography (rectovaginography).
● To adapt to functional dysfunctional outlet constipation, i.e. the desire to defecate, the desire to stop, the constant feeling of not being able to defecate. Preoperative preparation: (1) Take barium sulphate 2-3 hours before the imaging (to fill up the last section of small intestine). (2) Clean enema 1-2 hours before imaging. (3) Contrast method: special simulated fecal contrast agent (70-75% water content, viscosity 245g), special pusher, dynamic filming under fluoroscopy.
●Diagnostic criteria: Diagnosis of the presence or absence of pelvic floor muscle dystrophy syndrome and pelvic floor muscle relaxation syndrome. For example: puborectal muscle hypertrophy, perineal descent, rectal mucosal prolapse, internal rectal intussusception, visceral prolapse and intestinal hernia, anterior proctosis of the rectum. Simulated faecography has clear advantages in the diagnostic imaging of the above diseases.
Colon Transmission Function Test: It is a test of colonic dynamics.
● Examination method: Prohibit taking laxatives 2-3 days before the examination, swallow 1 capsule containing an X-ray impermeable marker after breakfast on the day of the examination, and take 3 plain films of the abdomen 24, 48, and 72 hours after taking them, respectively.
●Measurement method: Drawing lines and zoning on the abdominal film, the abdomen was divided into three zones: the right colon zone, the left colon zone, and the b-rectal zone. Compare the distribution of markers in each region. Types of colon slow transmission are common in patients with constipation, slow transmission in the b-rectal region, slow transmission in the left colon, slow transmission in the right colon, and mixed slow transmission.
Colon gas-barium double contrast imaging.
A cleansing enema is performed 1 to 2 hours before the examination, and then the examination is performed in the radiology department. Barium enema is mainly used for primary constipation caused by sigmoid colon redundancy, colonic tumour, congenital megacolon and other factors.
In conclusion, for various types of constipation should choose different examination methods, also can choose the joint application of two examination methods, specific problems specific analysis. We welcome all constipation patients to visit our department.

Specialists are carefully examining the patients without pain.


Figure 1 Figure 2
Case 1 Figure 1: The patient has been suffering from constipation for 10 years, 48 hours after taking the capsule containing the marker, the film shows that most of the marker lines are located in the left half of the colon, especially in the splenic region.
Case 1, Figure 2: 72 hours after taking the capsule containing the marker, the film was reviewed and it was seen that the markers were still mostly located in the left half of the colon, with the splenic region being prominent and slow transmission in the left half of the colon.

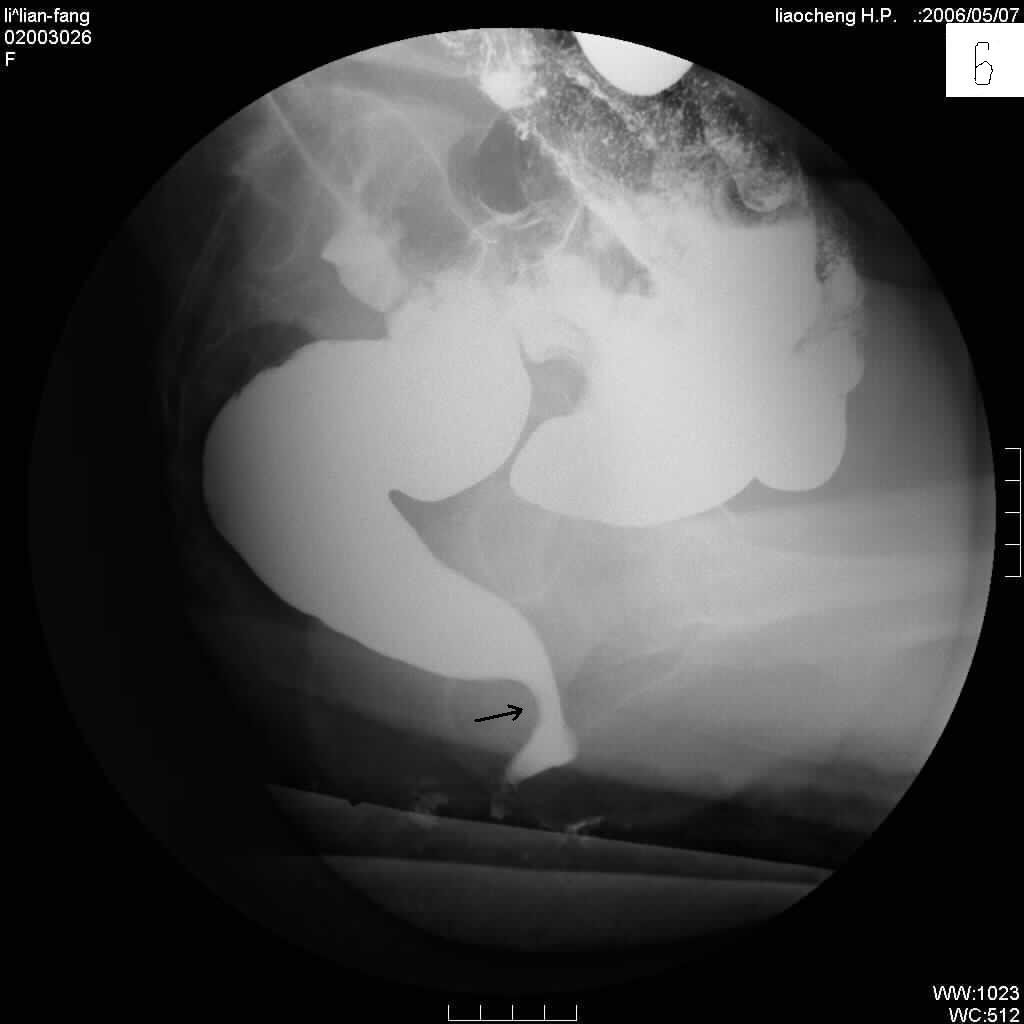
Figure 3 Figure 4
Case 1 Figure 3: Review of the film 96 hours after administration of the capsule containing the marker showed that most of the marker was located in the sigmoid region. Functional dysfunctional outlet disease is considered and a simulated rectal fecography is appropriate.
Case 2 Figure 4; Simulated rectal fecography image with the lower thick black arrow pointing to the anterior portion of the rectum. The thin black arrow in the upper part refers to an accidentally detected rectal cancerous lesion.

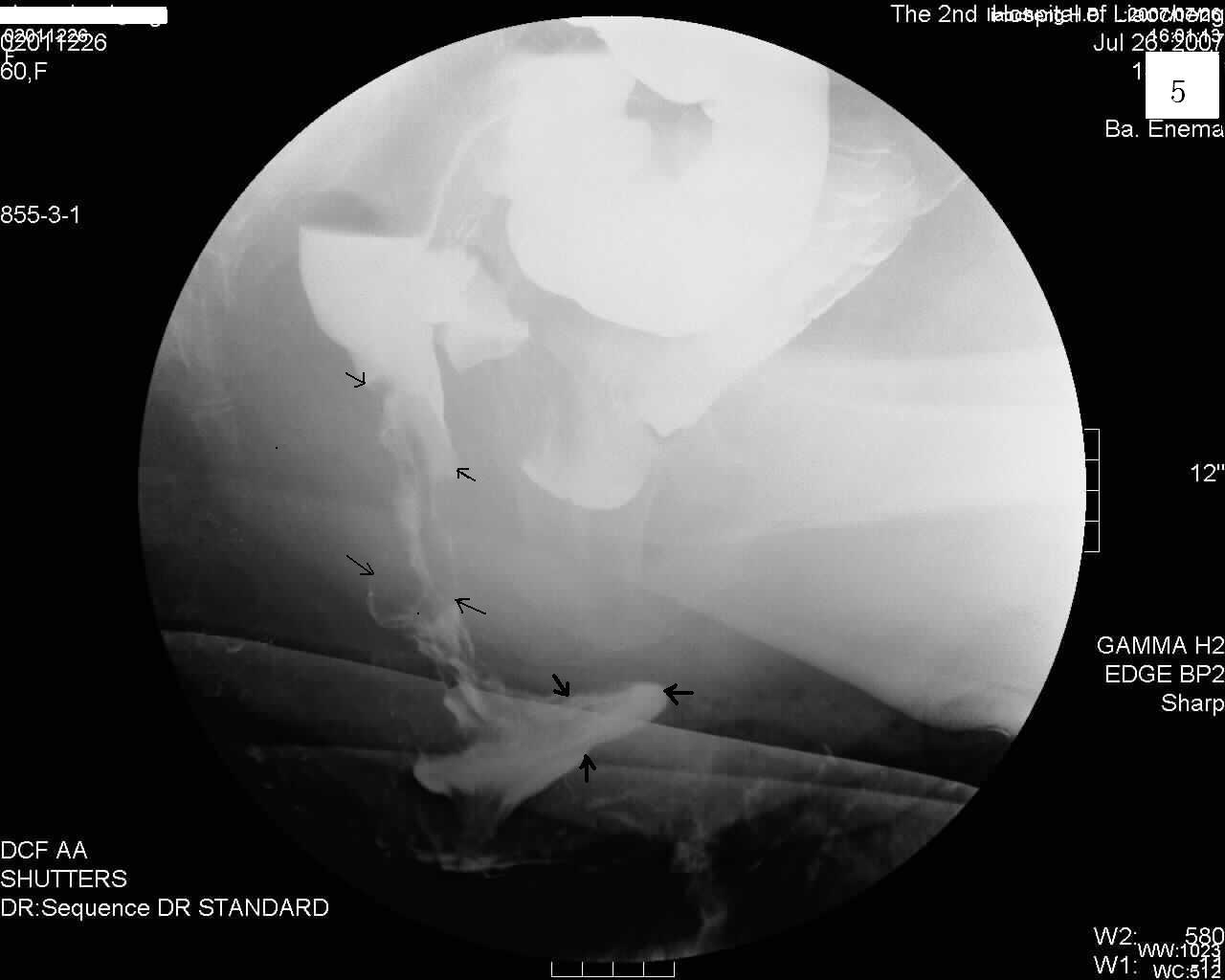
Figure 5 Figure 6
Case 3 Figure 5; shows a simulated rectal voiding contrast image, the part of the image indicated by the arrow is the deep part of the anterior rectal protrusion.
Case 4 Figure 6: Simulated rectal defecation contrast image of the posterior part of the rectum with the arrow pointing to the hypertrophy of the puborectal muscle, which is causing difficulty in defecation.


Figure 7 Figure 8
Case 5 Figure 7 shows a sigmoid hernia in the black arrow portion. The white arrow portion is a posterior rectal mucosal prolapse. The yellow arrowed portion is the anterior rectal protrusion portion.
Case 6 Figure 8.9; Anterior rectal protrusion with posterior rectal mucosal prolapse force-row filling image and mucosal image.


Figure 9 Figure 10
Case 7 Figure 10; the part of the small intestine indicated by the white arrow is herniated.
Consultation with specialists: Zheng Dexian 13869572909
Ge Yinglin 13561291456
Tel: 0635-2342333
Nipple Excess and Mammary Ductography
During non-pregnancy and non-lactation period, fluid coming out when squeezing the nipple is called nipple discharge. Nipple discharge is one of the common symptoms of breast diseases. There are many diseases that can cause nipple discharge, which are summarised as three kinds of diseases: benign and malignant tumour; inflammation; and breast hyperplasia. Tumour accounts for 60-70%, of which breast cancer is about 26.7%. Especially the bloody overflow should be more alert to breast cancer, symptoms should be timely to the hospital.
Mammography is an examination method that injects a contrast medium into the milk ducts and then takes a film to show the ductal lesions. Mammography is a simple and safe method of screening patients with non-lactating overflow and is the most important method of detecting early breast cancer with overflow as the main symptom.
Indications:
1, For patients with abnormal or pathological nipple overflow: including bloody, plasma, yellow and clear watery nipple overflow, etc. It is especially suitable for single-hole overflow.
2、For any bilateral nipple overflow during non-pregnancy and lactation, those who exclude pituitary tumour; or unilateral nipple overflow, no matter whether the overflow is plasma, bloody, milky, pasty, coloured or colourless; all of them should undergo mammary ductography to diagnose the lesions of the mammary ducts and their surrounding tissues.
3、Any non-pregnant, non-lactating nipple overflow, or nipple overflow beyond the normal duration of lactation, whose lesion cannot be shown by X-ray film.
4, For some breast cancer patients, although there is no nipple overflow, can also be performed breast ductography.
Contraindications:
1. patients suffering from acute mastitis;
2. pregnancy is a relative contraindication, pregnant women should cover their abdomen with a lead skirt if they have to undergo breast ductography.
3. allergy to contrast media
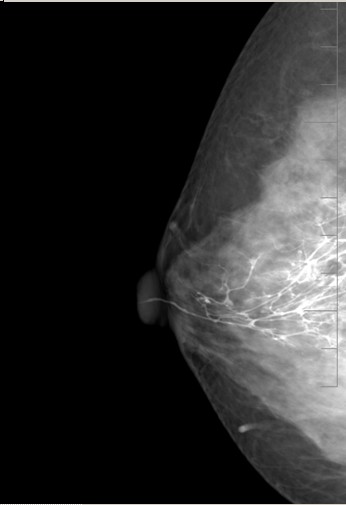

Normal Ductography Film Dilated Mammary Ducts Breast Overflow
You know what? Dry mouth and dry eyes are also diseases
--Clinical application of parotid imaging techniques
In daily life, some people probably feel discomfort such as dry mouth and dry eyes, is this a disease? And what kind of disease could it be? People with such symptoms may be suffering from the disease of dry syndrome, and should go to the hospital for examination and treatment in time.
Dryness syndrome is a systemic autoimmune disease that involves the oral cavity where the salivary glands open, and dryness is an important clinical manifestation. Parotid imaging is an important indicator that can reflect the functional and morphological involvement of the parotid glands, and is regarded as the gold standard for the diagnosis of parotid ductal lesions.
Parotid angiography is a method of examination in which a contrast medium is injected into the parotid duct through the opening of the parotid gland to show the condition of the parotid duct and its surrounding tissues. It can be used to diagnose dry syndrome, chronic inflammation of the parotid gland, tumours, and whether the surrounding tissue of the parotid gland has invaded the gland.

Dry Syndrome Patient Movie
Consultation Specialist: Li Guihua 13666382963
Zheng Dexian 13869572909
Department Tel: 0635-2342675
0635-2342334



 鲁ICP备11009722号-4
鲁ICP备11009722号-4 